C2.3 Spirometry
The diagnosis of COPD rests on the demonstration of airflow limitation which is not fully reversible (Global Initiative for Chronic Obstructive Lung Disease 2017) [evidence level II].
It is important in general practice settings to obtain accurate spirometric assessment (Walters 2011b) [evidence level III-3].
Because COPD is defined by demonstration of airflow limitation which is not fully reversible, spirometry is essential for its diagnosis (see Figure 4) and this may be performed in the community or prior to discharge from hospital (Rea 2011). Most spirometers provide predicted (“normal”) values obtained from healthy population studies, and derived from formulas based on height, age, sex and ethnicity.
Airflow limitation is not fully-reversible when, after administration of bronchodilator medication, the ratio of FEV₁ to forced vital capacity (FVC) is <70% and the FEV₁ is <80% of the predicted value. The ratio of FEV₁ to vital capacity (VC) is a sensitive indicator for mild COPD. FEV₁/FEV6 has a high level of agreement with FEV₁/FVC on both the fixed ratio and Lower Limit of Normal (LLN) criteria for the diagnosis of COPD (Bhatt 2014a). There is controversy regarding the optimal cut-off to define airflow limitation (FEV₁/FVC less than 0.7 versus lower limit of normal). There is evidence that the fixed ratio can lead to over diagnosis of COPD in older populations, under diagnosis in younger people (Cerveri 2008, Vollmer 2009, Swanney 2008) and may lead to gender imbalances as women have higher FEV₁/FVC than their male counterparts (Guerra 2009). A systematic review of 11 studies which examined the relationship of each criterion with clinical outcomes found both were related to clinical outcomes and concluded that on current evidence one could not be preferred over the other. The LLN appeared to be a better criterion in older patients with less severe airflow limitation (van Dijk 2014); however a study (Bhatt 2014b) shows that the fixed cut-off of 0.7 identified more people with CT diagnosed emphysema.
In 2022, the ERS/ATS technical standard on interpretive strategies for routine lung function tests recommended using z-scores (e.g. Global Lung Initiative equations) as a diagnostic tool for COPD (Stanojevic 2022). Z-scores express how far an observed value is from predicted value after accounting for age, sex, height, and ethnicity in standard deviations. The 5th and 95th percentile limits (−1.645 and +1.645 z-score) of the healthy population can be used to identify individuals with spirometry results outside of the normal range.
A large and comprehensive study investigated the use of z-scores to identify individuals at high risk of developing COPD and other chronic lung diseases (Dharmage 2023) [evidence level III-2]. The findings of this study demonstrate how z-scores may be a valuable tool for improving early detection (Dharmage 2023; see section C1.1).
However, there are a number of limitations to the use of z-scores for COPD diagnosis. First, z-scores are not as well validated as percent predicted values. Second, selecting the appropriate reference equation that considers an individual’s sex, geographic, and ancestral background is complicated and can introduce uncertainty to interpreting their z-scores. Furthermore, risks associated with misdiagnosis and misclassification from fixed ratio thresholds are low, especially when spirometry is used in conjunction with other clinical indicators of COPD-like symptoms. Given the limitations of z-scores and the low risks and clinical convenience of the fixed ratio criteria, fixed ratio criteria remain the preferred method for COPD diagnosis in the COPD-X and GOLD 2023 guidelines (GOLD 2023).
Concerning healthcare utilisation and COPD mortality, a population-based study of 11, 077 adults in the US found that an FEV₁/FVC ratio of <0.70 identified individuals who were at risk of COPD hospitalisations and COPD-related mortality, with equal or better accuracy than other ratios ranging from 0.75 to 0.65, and with more accuracy than the lower limit of normal (Bhatt 2019) [evidence level III-2]. This study supported using the fixed FEV₁/FVC ratio of <0.70 to identify individuals at risk of clinically significant COPD.
Figure 4: Comparison of flow-volume curves for spirometry
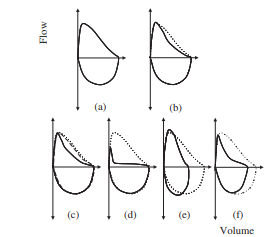
The dotted line for all curves represents a normal flow–volume curve in a young adult. (a) and (b) depict typical flow–volume curve shapes for spirometry within normal limits for a young adult and older person, respectively. Note that the expiratory limb of (b) has some concavity despite the result being within normal limits. (c) shows an example of airway obstruction with almost complete reversibility. The baseline curve (solid line) has concavity, typical of airflow obstruction. The post-bronchodilator curve (dashed line) has returned to close to the ‘normal’ curve (dotted). (d) depicts significant airflow obstruction. (e) represents the pattern often seen with restriction. The curve appears to be compressed along the volume axis, but the expiratory limb does not appear to have any concavity. (f) portrays an obstructive pattern. Note also that the volume appears to be reduced. This pattern may represent obstruction with a reduced FVC due to gas trapping or may represent a mixed obstructive/restrictive ventilatory pattern. Measurement of static lung volumes are required for determination.
(Figure reproduced from Interpreting Lung Function Tests: A Step-by-Step Guide, First Edition. Brigitte M. Borg, Bruce R. Thompson and Robyn E. O’Hehir. © 2014 John Wiley & Sons, Ltd. with permission from Wiley)
A detailed systematic review states that spirometry, in addition to clinical examination, improves the diagnostic accuracy of COPD compared to clinical examination alone reinforcing the importance of spirometry (Wilt 2005) [evidence level I]. The current inaccuracy of diagnosis in community settings and the importance of using spirometry was demonstrated by an Australian study where only 58% of general practice patients being treated for COPD were confirmed to have the diagnosis on post-bronchodilator spirometry (Zwar 2011). The unreliability of clinical assessment for the diagnosis of COPD has also been shown in a study in Dutch primary care (Lucas 2012). More studies are required to define any benefit from the use of spirometry for case finding in COPD, and to evaluate the effects of spirometric results on smoking cessation.
The spirometric tests require high levels of patient effort and cooperation, and there are important quality criteria that should be met in conducting spirometry (Miller 2005).
Indications for spirometry include:
- breathlessness that seems inappropriate;
- chronic (daily for two months) or intermittent, unusual cough;
- frequent or unusual sputum production;
- relapsing acute infective bronchitis; and
- risk factors such as exposure to tobacco smoke, occupational dusts and chemicals, and a strong family history of COPD.
There is evidence of both underdiagnosis (Toelle 2013) and misdiagnosis of COPD in the community (Zwar 2011). In a community-based study of 1615 participants with a range of respiratory symptoms, but not recalling a diagnosis of respiratory disease, 8.4% had spirometry results consistent with asthma and 12.1% subjects had spirometry results consistent with COPD (Alhabeeb 2022). This highlights the prevalence of undiagnosed airways disease. These undiagnosed subjects also had more severe respiratory symptoms as assessed by the COPD Assessment Test (CAT), and poorer health-related quality of life as assessed by the St. George’s Respiratory Questionnaire (SGRQ) compared to subjects with no airflow obstruction. This study highlights a beneficial yield of airways disease diagnoses, in adults who have respiratory symptoms but without a diagnosis, by performing spirometry.
In a systematic review examining under and overdiagnosis in primary healthcare settings Perrett et al (2023) found that based on evidence from three studies of symptomatic smokers the prevalence of spirometry-confirmed COPD without a diagnosis documented in their health records was 14%–26%. The same review found substantial evidence of misdiagnosis. Based on four case series of COPD diagnosed documented in primary healthcare records, only between 50% and 75% of subjects had airflow obstruction on postbronchodilator spirometry performed by study researchers (Perret 2023) [evidence level III-1]. In a general practice setting, patients with comorbidities may be more commonly mis-diagnosed with COPD. In a study of 1,050 smokers or ex-smokers identified from 41 Melbourne general practices, two-thirds were current smokers (Liang 2018). More than one-third of participants with a prior diagnosis of COPD did not meet the spirometric definition of the disorder. 1 in 6 participants not previously diagnosed with COPD had spirometry test results consistent with COPD. Spirometric assessment is important in these patients to minimise this risk (Zwar 2011). Two pulmonologists reviewed 333 patients with physician-diagnosed COPD and/or asthma. The patients had two or more emergency room visits or admissions over the preceding 12 months, with prospective evaluation over the next 10 months. The study found that a third of these patients had neither asthma nor COPD, and a quarter may not even have any form of airflow limitation. The study highlighted the importance of spirometry in making the correct diagnosis, which had been performed in less than a third of the patients studied (Jain 2015). Respiratory symptoms are of clinical importance even in those current or former smokers with preserved lung function (Woodruff 2016). Further evidence is required for optimal management of these patients.
Inaccurate diagnosis related to lack of use of spirometry is also an issue in the hospital setting. Habteslassie et al (2021) conducted a retrospective audit of inpatient separations in one Victorian hospital. A total of 2239 inpatient separations occurred in 1469 individuals who had a clinical diagnosis of COPD in the period October 2016 to March 2018. Spirometry results were not available in 43.6% (n = 641) of the sample and a further 19.7% (n = 289) had spirometry results available at the time of admission that did not demonstrate fixed airflow obstruction. The authors noted the risks of inappropriate treatment related to the lack of diagnostic accuracy.
In a Danish study (Katsimigas 2019) of case finding for COPD carried out in symptomatic smokers and ex-smokers (n=6,710), BMI <25 kg/m2 and BMI >35 kg/m2, increasing age and an increasing number of pack-years smoked were all important predictors for COPD (diagnosed in 17.7% in this study). GPs should target these patients for case finding to facilitate early diagnosis and initiate early interventions.
Aaron et al (2017) studied two longitudinal cohorts of patients with mild to moderate COPD on post-bronchodilator spirometry at baseline and found that transient episodes of diagnostic instability occurred commonly and that 12 to 27% of patients reversed their diagnosis of COPD over a 4 to 5 year period. Diagnostic reversal was most common for patients who quit smoking during the study period. These findings suggest there is considerable variability of spirometry results around the FEV₁/FVC threshold and that a single spirometric assessment may not be reliable for diagnosing COPD in patients with mild to moderate airflow limitation. If spirometry results are around the threshold, repeat spirometry should be performed to confirm diagnosis.
< Prev Next >

