X: Manage eXacerbations
Key Recommendations for X: Manage eXacerbations | LoE | SoR |
|---|---|---|
| Diagnose a COPD exacerbation based on changes in the patient’s baseline dyspnoea, cough, and/or sputum that exceed normal day-to-day variations, are acute in onset, and may warrant a change in regular medication or hospital admission | III-2 | Strong |
| Diagnosing and treating exacerbations early may prevent hospital admission and delay COPD progression | III-2 | Strong |
| Initiate inhaled short-acting bronchodilators as a first-line treatment of exacerbations | I | Strong |
| Consider prescribing systemic corticosteroids to reduce the severity of and shorten recovery from exacerbations (oral route, when possible; 30 to 50mg daily for 5 days) | I | Strong |
| Consider prescribing antibiotic therapy (amoxycillin or doxycycline for 5 days) for COPD exacerbations with clinical features of infection (increased volume and change in colour of sputum and/or fever) | I | Strong |
| Use supplemental oxygen for hypoxaemia in COPD exacerbations, target SpO₂ 88% to 92% to improve survival | II | Strong |
| Controlled oxygen delivery (0.5 to 2.0 L/min) is indicated for hypoxaemia in patients with exacerbations. | II | Strong |
| Non-invasive ventilation improves survival for people with COPD and acute hypercapnic respiratory failure | I | Strong |
| Refer to pulmonary rehabilitation, particularly during the recovery phase following an exacerbation | I | Strong |
| The primary healthcare team should ensure that patients with COPD receive comprehensive follow-up care, after they are discharged from hospital following an exacerbation | I | Strong |
| Coordinate multidisciplinary support to help treat COPD exacerbations for patients in the community setting receiving home management | I | Weak |
| LoE = Level of evidence according National Health and Medical Research Council (NHMRC) Evidence Hierarchy according to type of research question (Box 1); SoR = Strength of recommendation according to the GRADE (Andrews 2013, Guyatt 2008) |
||
EXACERBATIONS of COPD which are more frequent in the winter months in temperate climates (Jenkins 2012) [evidence level II] often require hospital admission for treatment of respiratory failure. A record linkage study in WA (Geelhoed 2007) demonstrated that the rate of hospital admission for COPD has been declining. The risk of readmission was highest within three months of discharge and more than half of all patients were readmitted within 12 months. About 10% of patients with a primary diagnosis of COPD died either during admission or within the same year. Median survival from first admission was five years in men and eight years in women. The poorest survival was among older patients with recognised emphysema. In one study of more than 1,000 patients admitted to several hospitals with an exacerbation of severe COPD, about 50% were admitted with a respiratory infection, 25% with congestive cardiac failure, and 30% with no known cause for the exacerbation (Connors 1996). A study of 173 patients with COPD reported an average of 1.3 (range 0 to 9.6) exacerbations annually. An ecological study of hospital admissions for COPD in Victoria found higher rates of admission in rural and remote areas with greater socioeconomic disadvantage and higher rates of smoking (Ansari 2007).
Exacerbations become more frequent as severity of COPD worsens (Hoogendoorn 2010a). In the study by the ECLIPSE investigators, exacerbation rate increased with increasing GOLD stage, such that 22% of patients with GOLD stage 2 disease had two or more exacerbations during one year of follow-up, whereas 47% of patients with GOLD stage 4 disease had frequent exacerbations over the same period. The single best predictor of exacerbations across all GOLD stages was prior exacerbations. Other predictors included a history of heartburn , poorer quality of life and elevated white cell count (Hurst 2010). ECLIPSE data also showed that a history of prior hospitalisation for COPD is the strongest predictor of subsequent hospitalisation. Han et al prospectively examined exacerbation rates in 1,105 patients with COPD over a three-year period from the SPIROMICS cohort (Han 2017). Contrary to the ECLIPSE study, Han reported that individual exacerbation rates vary significantly from year to year, and very few patients experience two or more exacerbations over successive years. In addition to a history of past exacerbations, Han reported that interleukin-15 (IL-15) and interleukin 8 (IL-8) levels in blood as well as small airway abnormalities on CT chest predicted frequent exacerbations (Han 2017).
The ECLIPSE data also confirmed 12-month mortality rates were significantly higher in patients hospitalised for COPD (15%) compared to those without hospitalisation (5%) (p<0.001) (Mullerova 2015). In a Spanish cohort of (predominantly male) patients prospectively followed, Guerrero et al demonstrated that re-admission to hospital within 30 days following discharge for an exacerbation of COPD increased 12 month mortality rates (37% in readmitted versus 17% in non-readmitted patients, p=0.001) and was an independent risk factor for mortality at one year (HR 2.48 95% CI 1.1-5.59) (Guerrero 2016).
Studies have confirmed that although the prognosis of exacerbations is poor, the prognosis post-exacerbation is improving. Hoogendoorn et al (Hoogendoorn 2010b) identified six cohort studies that followed the survival of COPD patients for at least 1.5 years after a severe exacerbation resulting in hospitalisation. A meta-analysis resulted in a weighted average case-fatality rate of 15.6% (95% CI 10.9-20.3). The excess risk of mortality continued after discharge from hospital. Almagro et al (Almagro 2010) prospectively examined three-year mortality after a severe exacerbation resulting in hospitalisation in two well matched cohorts seven years apart (1996/97 and 2003/04). The 1996/97 three-year survival rate was 53% and the 2003/4 three-year survival rate was significantly improved at 61% (log rank p = 0.017). The 2003/4 cohort had increased usage of tiotropium, long acting beta2 agonists, angiotensin receptor blockers, statins and anti-platelet therapy. The authors speculated that the increased survival may be due to improved treatment options for COPD and co-morbidities including cardiac disease [evidence level III-2].
Soltani et al (Soltani 2015) prospectively evaluated a cohort of 150 severe COPD patients admitted with an exacerbation of COPD at an Australian tertiary hospital and reported a 28% readmission rate at three months and a 12 month mortality rate of 24.5%. It should be noted that patients requiring invasive or non-invasive ventilation were excluded from this study. A retrospective database study of over 2 million COPD admissions among American Medicare recipients above the age of 65 reported a 12 month mortality rate of 26.2% (Lindenauer 2018). The 12 month mortality rate for those requiring invasive and non-invasive ventilation was 45.7% and 41.8% respectively. This study showed a 12 month readmission rate of 64% (Lindenauer 2018). Analysis of over 1 million COPD admissions from a US national database that included patients of all age groups and all healthcare providers demonstrated a 19.2% 30 day readmission rate (Jacobs 2018). A systematic review of over 40 studies reported a 30-day COPD related readmission rate of 11% and a 12-month readmission rate of 37% (Ruan 2023) [evidence level III-2].
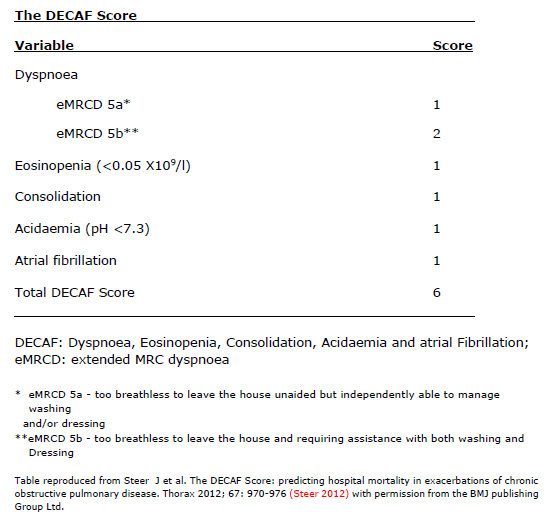
DECAF (see Box 12) is a 30-day mortality prediction score for COPD admissions (Steer 2012). DECAF was derived with data from 920 consecutive patients admitted with a COPD exacerbation from two neighbouring hospitals in the UK. COPD had been confirmed on spirometry. The five strongest predictors of mortality that comprise the score are extended MRC Dyspnoea Score, eosinopenia, consolidation, acidaemia, and atrial fibrillation. The score showed high discrimination for mortality with an area under the receiver operator characteristic curve = 0.86, 95% CI 0.82 to 0.89. A DECAF score of 3 predicts confers a 27.2% 30-day mortality risk. Echevarria et al examined the performance of the DECAF score in 2,645 patients with an admission of COPD across 6 hospitals in the UK and reported a similarly high performance for mortality prediction (Echevarria 2019).
Box 12. The Dyspnoea, Eosinopenia, Consolidation, Acidaemia and atrial Fibrillation (DECAF) score
In patients with COPD the normally sterile lower airway is frequently colonised by Haemophilus influenzae, Streptococcus pneumoniae and Moraxella catarrhalis. While the number of organisms may increase during exacerbations of COPD, the role of bacterial infection is controversial (Macfarlane 1993, Smith 1980, Soler 1998, Wilson 1998, Stockley 2000, Walsh 1999, Mogulkoc 1999, Murphy 1999, Miravitlles 1999). Exacerbations can also be caused by viral infection (Seemungal 2001). Retrospective data from an Australian tertiary hospital demonstrated that influenza virus and rhinovirus were the most common viral pathogens found in patients admitted to hospital with an exacerbation of COPD (Biancardi 2016). Given the current COVID-19 pandemic, it is recommended that patients with COPD take adequate precautions to stay well (https://lungfoundation.com.au/lung-health/protecting-your-lungs/coronavirus-disease-covid-19/what-you-need-to-know/). Guidance for diagnosis and management of COVID-19 infection is highly relevant to patients with COPD. Living guidelines from the National COVID-19 Clinical Evidence Taskforce are available at https://covid19evidence.net.au/#living-guidelines.
Other causes of exacerbations of COPD include left ventricular failure and pulmonary embolus (PE). A systematic review comprising seven studies with a total of 880 patients who were hospitalised with an exacerbation of COPD and underwent a CT pulmonary angiogram (CTPA) found that 16% had a PE (Aleva 2017). There was large variation in the prevalence of PE between studies (3% to 29%). One third of patients had only small, isolated, sub-segmental PE. A prospective study of 740 patients with COPD with an acute worsening of respiratory symptoms presenting to 7 French hospitals found a prevalence of 5.9% of PE on CTPA, based on a predefined diagnostic algorithm including clinical probability based on the Geneva score and D-dimer testing (Couturaud 2021). A diagnosis of PE should be considered in patients presenting with an exacerbation of COPD when signs of respiratory infection are absent, and chest pain or cardiac failure are present.
A panel study of patients with moderate to severe COPD demonstrated that exacerbations could also be triggered by urban air pollutants such as PM10, black smoke and NO2 (Peacock 2011) [evidence level II]. Chest trauma and inappropriate use of sedatives can lead to sputum retention and hypoventilation.
Prolonged COPD exacerbations are associated with worse health status and the exacerbation that follows occurs sooner. Exacerbations of COPD are associated with accelerated loss of lung function, particularly in patients with mild disease. In patients with mild COPD each severe exacerbation was associated with an additional FEV1 loss of 87 ml/year (95% CI 23 to 151) (Dransfield 2017). Retrospective analysis of data from the UPLIFT study also demonstrated an accelerated loss of lung function after a single COPD exacerbation (Halpin 2017).
Early diagnosis and prompt management of exacerbations of COPD may prevent progressive functional deterioration and reduce hospital admissions (Lorig 1999, Shepperd 1998). Education of the patient, carers, other support people and family may aid in the early detection of exacerbations. A self-management plan developed in conjunction with the patient’s GP and specialist to indicate how to step-up treatment may be useful (see examples at https://lungfoundation.com.au/resources/?search=action%20plan). This plan might indicate which medications to take, including antibiotics and oral corticosteroids. The plan should also require patients to contact their GPs or community nurses to allow rapid assessment (see section D).
Statins have been shown to reduce rates of hospitalisation (for COPD or any other reason), lung-function decline, the need for mechanical ventilation, and all-cause mortality in observational studies of COPD patients. The Prospective Randomized Placebo-Controlled Trial of Simvastatin in the Prevention of COPD Exacerbations (STATCOPE) examined the effect of daily treatment with simvastatin in patients with moderate-to-severe COPD who were at high risk for exacerbations and had no other indications for statin treatment. Simvastatin at a daily dose of 40 mg for at least 12 months did not affect exacerbation rates or the time to a first exacerbation (Criner 2014) [evidence level II].
Hospital admissions are indicators or failed prevention and are highly expensive to health care systems. Hospitalisations are being included increasingly as an outcome measure in randomised controlled trials of a range of interventions. Box 13 summarises the interventions that have been demonstrated, in such randomised control trials to statistically significantly reduce hospitalisations.
| Level of Evidence | Intervention | Demonstrated impact | Effect Estimate | COPD-X Section | Citation |
|---|---|---|---|---|---|
| Level I | LAMAs | “…LAMAs had reduced exacerbation rates…and exacerbation-related hospitalisations…compared to LABAs” NB: most participants in this analysis had Tiotropium as their LAMA | 22% improvement (RR 0.78, 95% CI 0.69 to 0.87) | O1.2.1 | Maia 2017 |
| Tiotropium | “… tiotropium reduced the odds of a COPD exacerbation … and related hospitalisations compared to placebo or ipratropium.” | 36% improvement (OR 0.64, 95% CI 0.51 to 0.82; NNT 30, 95% CI 22 to 61) | P5.1 | Barr 2005 | |
| "… tiotropium was more effective in preventing COPD exacerbations leading to hospitalisation [compared to a range of other LABAs]” | 14% improvement (OR 0.86, 95% CI 0.79 to 0.93) | P5.2 | Chong 2012 | ||
| Aclidinium | “…Aclidinium resulted in marginal improvements in quality of life and FEV1, and reduced the number of patients with exacerbations requiring hospitalisation” | NNT 77, 95% CI 51 to 233 | O1.2.1 | Ni 2014 | |
| Systemic corticosteroids | “… systemic corticosteroids reduce treatment failure (defined as additional treatment, hospital admission/re-admission for index episode, return to emergency department, unscheduled physician visit for the index episode), improve lung function, shorten recovery and reduce the severity of exacerbations of COPD … reduced the risk of treatment failure by over half compared with placebo in … median treatment duration 14 days” | 52% improvement (OR 0.48, 95% CI 0.35 to 0.67 NNT 9) | X2.2.2 | Walters 2014 | |
| Non-invasive ventilation | “The use of NIV reduces hospital length of stay.” | MD -3.39 days, 95% CI -5.93 to -0.85 | X3.2 | Osadnik 2017 | |
| Hospital at home | “… compared to standard care, participants allocated to hospital in the home were significantly less likely to be readmitted to hospital within the next 1 to 6 months.” | 24% improvement (RR 0.76, 95% CI 0.59 to 0.99) | X1 | Jeppesen 2012 | |
| Multi-faceted care plans | “… integrated disease management programs defined as ‘a group of coherent interventions designed to prevent or manage one or more chronic conditions using a systematic, multidisciplinary approach and potentially employing multiple treatment modalities.’ … found positive effects on disease-specific QoL … exercise tolerance, hospital admissions and hospital days per person…” | Admissions: 32% improvement (OR 0.68, 95% CI 0.47 to 0.99 NNT 15) Length of stay: MD -3.78 days, 95% CI -5.90 to -1.67 | D3 | Kruis 2013 | |
| Pulmonary rehabilitation | “Pulmonary rehabilitation following hospitalisation for an exacerbation also reduced hospital readmissions.” | 56% improvement OR 0.44, 95% CI 0.21 to 0.91 | X3.6 | Puhan 2016 | |
| Level II | LAMA/LABA/ICS (umeclidinium/ vilanterol/ fluticasone furoate) | “In selected COPD patients with a history of exacerbations there was a 34% reduction in admissions with triple therapy using a single inhaler (fluticasone [ICS], vilanterol, umeclidinium – IMPACT study), as well as other benefits, regardless of baseline bronchodilator responsiveness, compared to dual therapy (no ICS), and with even greater benefits in some outcomes demonstrated in those with high eosinophil counts (>150 cells/ microlitre).” | 34% improvement (RR 0.66, 95% CI 0.56 to 0.78) | O4.2.1 | Lipson 2018 |
| Airway clearance techniques | “The use of ACTs was associated with a significant short-term reduction in the need for increased ventilatory assistance … duration of ventilatory assistance …and hospital length of stay.” | MD - 0.75 days, 95% CI -1.38 to -0.11 | X3.4 | Osadnik 2012 | |
| Discharge bundles | “… the use of COPD discharge bundles reduced hospital readmissions …” | 20% improvement (RR 0.80, 95% CI 0.65 to 0.99) | X3.7 | Ospina 2017 | |
| Supported discharge programs & medication adherence | “…has been shown to reduce re-admissions for COPD exacerbations compared to usual care …” | 45% improvement (HR 0.55, 95% CI 0.35 to 0.88) | X3.8 | Casas 2006 | |
| “Adherence to inhaled medication regimes is associated with reduced risk of death and admissions to hospital due to exacerbations in COPD...” | 44% improvement (RR 0.56, 95% CI 0.48 to 0.65) | O | Vestbo 2009 | ||
| Nurse-led and allied health-led self-management programs | “Lowered mortality, and reduced emergency and emergent hospitalisation” | 16% improvement (HR 0.84, 95% CI, 0.78-0.90) 8% improvement (IRR 0.92, 95% CI, 0.86-0.98) 11% improvement (IRR, 0.89, 95% CI, 0.83-0.95). | D3 | Wang 2024 | |
| ACTs = Airway Clearance Techniques; CI = Confidence Interval; COPD = Chronic Obstructive Pulmonary Disease; HR = Hazard Ratio; ICS = Inhaled Corticosteroids; LABAs = Long-Acting Beta Agonists; LAMA = Long-Acting Muscarinic Antagonists; LAMA/LABA/ICS = umeclidinium/vilanterol/fluticasone furoate; MD = Mean Difference; NIV = Non-Invasive Ventilation; NNT = Number Needed to Treat; OR = Odds Ratio; RR = Relative Risk. Summary of Level I and Level II evidence for interventions shown to reduce hospitalisations in patients with COPD. |
|||||


